Abstract
Sirtuin-1 (Sirt-1), NAD-dependent histone deacetylase, plays a crucial role in various biological processes including cellular senescence, metabolism and inflammatory responses. Sirt-1 deacetylation regulates different transcription factors that are important for modulating immune responses. An early study showed that Sirt-1 is required to maintain T cell tolerance, but more studies provided evidences that Sirt-1 promotes Th17 responses while inhibiting function of Foxp3+regulatory T cells (Tregs). Thus, the question still remains as how Sirt-1 regulates T-cell immunity versus tolerance.
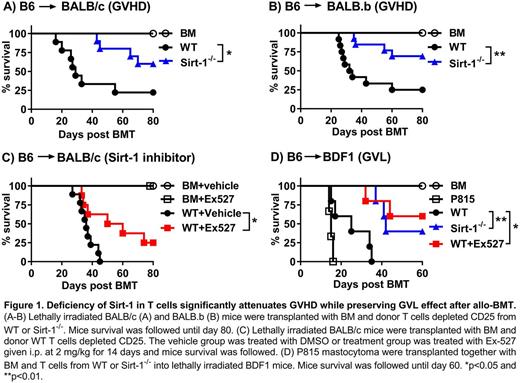
Graft-versus-host-disease (GVHD) remains one of the major complications after allogeneic bone marrow transplantation (allo-BMT). In the current study, we address the role of Sirt-1 in T-cell responses to alloantigens and in the induction of GVHD taking advantages of Sirt-1 conditional knock-out (Sirt-1fl/flCD4Cre) mice on C57BL/6 (B6) background. Using MHC mismatched (B6 to BALB/c) and MHC matched (B6 to BALB.b) murine BMT models, we observed that CD25-depleted Sirt-1-/- T cells significantly reduced their ability to induce acute GVHD compared to WT T cells, as the survival and clinical scores of the mice received Sirt-1-/- T cells were remarkably improved (Fig.1A-B). Importantly, more induced Tregs (iTregs, CD4+Foxp3+) were generated from Sirt-1-/- donor T cells than from WT counterparts in recipient spleen and liver 14 days after allo-BMT. Furthermore, Sirt-1-/- donor T cells significantly reduced IFN-γ production by both CD4 and CD8 T cells in vivo . Consistently, the levels of IL-4 and IL-10 cytokines in mice serum were significantly increased in mice transplanted with Sirt-1-/- T cells in parallel with the reduction of pro-inflammatory cytokines, IFN-γ and TNF-α. Altogether, the data suggests that Sirt-1 positively regulates T cell activation, proliferation and essential for GVHD induction.
We extend our study further into chronic GVHD pathophysiology, which is mainly driven by pathogenic CD4 T and B cells. We observed that splenocytes from Sirt1-/- donor remarkably reduced the clinical manifestation of cGVHD in recipient mice. Mechanistic studies revealed the significant increase of splenic B cell reconstitution with down regulation of B cell activation markers (CD86 and MHCII). Importantly, the frequency of follicular regulatory T cells (Tfr) was dramatically increased, which is known to play a critical role in suppressing T follicular helper (Tfh) and plasma B cell differentiation. Consistently, we observed a significant reduction of plasma B cell frequency in spleen of Sirt-1-/- group. Finally, we evaluated Sirt-1 as a therapeutic target by testing a specific inhibitor (Ex-527) in viv o. Using a haploidentical (B6 to BDF1) BMT model with P815 mastocytoma, we found that not only could Ex-527 significantly alleviate GVHD severity but also maintaining graft-versus-leukemia (GVL) activity against P815 tumor (Fig.1C-D). In conclusion, Sirt-1 is a promising therapeutic target for the control of aGVHD and cGVHD pathogenesis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.